ACTION RELATED TO CARE OF PATIENT
VENIPUNCTURE
Venipuncture means the collection of blood from a vein. As a general rule, arm veins are the best source from which to obtain blood. The preferred site is the antecubital fossa, which is where the arm bends at the elbow. The vein of choice is the median cubital vein (see figure).
The cephalic vein is not preferred because it has a tendency to roll but can be used as an alternative to the median cubital vein.
The basilic vein lies close to the brachial nerve and artery, and for this reason should be avoided.
In unusual situations, it may be necessary to use hand or wrist veins when a suitable arm vein cannot be located, or if the arms are bandaged or have been punctured repeatedly and are sore. Veins from the underside of the wrist should not be used.
Arterial punctures!!!
Do not attempt arterial punctures unless you have been properly trained and competency has been established. Always follow your institution’s policies and procedures.
Possible risks
- Arteries are not puncture because of the high pressure of blood in the vessels which consequently can lead to rapid bleeding and thrombi formation upon puncture.
- Sometimes, if the arm veins are used for repeated injection of fluids, they may be thrombosed. Thrombosis means that clots have formed and blood no longer flows. Thrombosed veins are usually firm, discolored, and tender. If the arm veins are thrombosed, you must use another site. Also, you should not obtain blood from a vein that has a hematoma (bruise) from a previous venipuncture.
- Repeated phlebotomy may result in anemia, and the patient may require a blood transfusion. Routine phlebotomy for 5 days usually results in the loss of 100 mL of whole blood, which can lower the hemoglobin by 0.48 to 1.02 g/dL and hematocrit by 1.3% to 2.5%. Conservation measures, such as the use of pediatric-sized blood collection tubes, can reduce this phlebotomy-related cause of anemia.
How the Test Will Feel
When the needle is inserted to draw blood, you may feel moderate pain, or only a prick or stinging sensation. Afterward, there may be some throbbing.
Why the Test is Performed
Blood is made up of two parts:
- Fluid (plasma or serum)
- Cells
Plasma contains various substances including glucose, electrolytes, proteins, and water. Serum is the fluid part that remains after the blood is allowed to clot in a test tube. Specifically, serum is the fluid part of blood after a substance called fibrinogen has been removed by clotting.
Cells in the blood include red blood cells, white blood cells, and platelets.
Blood helps move oxygen, nutrients, waste products, and other materials through the body. It helps control body temperature, fluid balance, and the body’s acid-base balance
Normal Results
Normal results vary with the specific test.
What Abnormal Results Mean
Abnormal results vary with the specific test.
INSTRUMENTS USED IN VENIPUNCTURE
A syringe is a simple pump consisting of a plunger that fits tightly in a tube. The plunger can be pulled and pushed along inside a cylindrical tube (called a barrel), allowing the syringe to take in and expel a liquid or gas through an orifice at the open end of the tube.
The open end of the syringe may be fitted with a hypodermic needle, a nozzle, or tubing to help direct the flow into and out of the barrel.
TOURNIQUET
 Tourniquet is a constricting or compressing device, specifically a bandage, used to control venous and arterial circulation to an extremity for a period of time. Pressure is applied circumferentially upon the skin and underlying tissues of a limb; this pressure is transferred to the walls of vessels, causing them to become temporarily occluded. It is generally used as a tool for a medical professional in applications such as cannulation or to stem the flow of traumatic bleeding, especially by military medics. The tourniquet is usually applied when the patient is in a life-threatening state as a result of continuous bleeding.
Tourniquet is a constricting or compressing device, specifically a bandage, used to control venous and arterial circulation to an extremity for a period of time. Pressure is applied circumferentially upon the skin and underlying tissues of a limb; this pressure is transferred to the walls of vessels, causing them to become temporarily occluded. It is generally used as a tool for a medical professional in applications such as cannulation or to stem the flow of traumatic bleeding, especially by military medics. The tourniquet is usually applied when the patient is in a life-threatening state as a result of continuous bleeding.
Applying tourniquet as below allow you to release the tourniquet quickly when the procedure is completed or if complications arises.
Note:Tourniquet that is too tight or applied for long period of time can block arterial blood flow which can lead to tissue or nerve damage
Safety tips on applying tourniquets
- Check to feel radial pulse, if cannot feel then the tourniquet is too tight
- Never leave a tourniquet in place for more than 2-3 minute
- If tourniquet was used in vein selection, release the tourniquet and wait for 2 minute before beginning the procedure and reapplying the tourniquet
What To Do if the Patient Feels Faints
Fainting does sometimes occur as a result of venipuncture. A patient may experience a feeling of weakness or light-headedness or in severe cases, the loss of consciousness at any time during the venipuncture procedure. Before the procedure. If a patient is aware that he/she gets light-headed, or has in the past fainted while having blood collected, the patient may alert the phlebotomist. The phlebotomist must then take appropriate measures to safeguard the patient during the procedure.
For example, the phlebotomist may instruct the patient to lie down instead of sitting upright during the procedure.This practice may lessen the risk of patient fainting and eliminate the possibility of patient injury due to falling or sliding out of a draw chair.
During the procedure If a patient faints during the venipuncture, immediately abort the procedure by gently removing the tourniquet and needle from the patients arm, apply gauze and pressure to the skin puncture site and call for assistance. If the patient is seated, place the patient’s head between his/her knees. A cold compress applied to the back of the neck may help to revive the patient more quickly. The use of an ammonia inhalant (smelling salts) to rouse the patient is considered an unsafe practice. The inhalant may cause irritation and/or anaphylactic shock in some patients. A typical fainting spell is self-limited and usually the patient comes around fairly quickly. However, the phlebotomist should stay with the patient for at least 15-30 minutes to ensure the patient has fully recovered from the fainting episode.
After the procedure If the patient states that he/she feels dizzy after the blood collection is completed, again, as stated above, place the patient’s head between his/her knees and apply a cold compress to the back of the neck. The phlebotomist should never direct the patient to an alternate location while the patient is experiencing dizziness. There is a great likelihood that the patient will faint while walking and be injured. It is never advisable for the phlebotomist to allow the patient to leave after the procedure until the patient is safely able to do so. It is important to review your facility’s specific procedures and know how to react appropriately if a patient experiences dizziness or faints during a blood collection.
CLEANING UP AFTER VENIPUNCTURE
During a blood collection, bacteria that is present on the skin surface may adhere to the outside of the needle as it enters into the vein. This can allow bacteria to infect the puncture site. A serious infection of the blood (septicemia) or of the tissue (cellulitis) may result. To avoid an infection, it is imperative that the phlebotomist uses a technique that thoroughly cleanses the skin at the site prior to venipuncture. Once the phlebotomist locates a suitable vein for venipuncture, the site of the vein that will be punctured is cleaned with a pre-packaged wipe saturated with 70% isopropyl alcohol. The site is cleansed using a “target” motion beginning at the center of the site and moving outward in concentric circles applying enough pressure to move surface bacteria away from the puncture point. It is not recommended to use a scrubbing back and forth motion to clean the site since you may drag bacteria from a dirty area back into the clean area. Allow alcohol to air dry for effective disinfection of the site. Never use non-sterile gauze to wipe dry the alcohol as this will contaminate the site. During the remainder of the procedure, the site must NOT be touched by anything that has not been cleaned in an identical manner. The phlebotomist should avoid retouching the site after cleaning. If it is absolutely necessary to re-palpate, the phlebotomist MUST clean the gloved finger in a manner identical to the above procedure. Make certain that no other piece of equipment touches the site. This includes ends of the tourniquet and gauze. If you suspect that your needle has touched the site before entry, dispose of the needle, re-clean the site and repeat the procedure using a new needle.
If a patient complains that there is redness or pain at the puncture site, even hours or days after the procedure, immediately refer the patient to his/her physician for evaluation.
VACUUM TUBES
 is a sealed glass or plastic tube from which air has been removed, the vacuum enhances automatic filling with blood according to pressure differences when needle is inserted into the vein and connected to vacuum tube
is a sealed glass or plastic tube from which air has been removed, the vacuum enhances automatic filling with blood according to pressure differences when needle is inserted into the vein and connected to vacuum tube
INTRAVENOUS THERAPY
Involves administering of fluids, nutrition, medication or blood products directly into the blood stream. About 90-95% of in patients receive some type of medication or fluid via I.V. line.
PURPOSE FOR I.V. INFUSION
- To provide parenteral nutrition
- To provide avenue for dialysis/apheresis
- To transfuse blood products
- To provide avenue for hemodynamic monitoring
- To provide avenue for diagnostic testing
- To administer fluids and medications with the ability to rapidly/accurately change blood concentration levels by either continuous, intermittent or IV push method.
The two main types of I.V. lines are peripheral and central lines
PERIPHERAL LINE
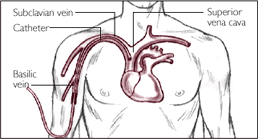
 A peripheral IV line (PVC or PIV) consists of a short catheter (a few centimeters long) inserted through the skin into a peripheral vein (any vein not inside the chest or abdomen). This is usually in the form of a cannula-over-needle device, in which a flexible plastic cannula comes mounted on a metal trocar. Once the tip of the needle and cannula are located in the vein the trocar is withdrawn and discarded and the cannula advanced inside the vein to the appropriate position and secured. Blood may be drawn at the time of insertion.
A peripheral IV line (PVC or PIV) consists of a short catheter (a few centimeters long) inserted through the skin into a peripheral vein (any vein not inside the chest or abdomen). This is usually in the form of a cannula-over-needle device, in which a flexible plastic cannula comes mounted on a metal trocar. Once the tip of the needle and cannula are located in the vein the trocar is withdrawn and discarded and the cannula advanced inside the vein to the appropriate position and secured. Blood may be drawn at the time of insertion.
Any accessible vein can be used although arm and hand veins are used most commonly, with leg and foot veins used to a much lesser extent. In infants the scalp veins are sometimes used.
with leg and foot veins used to a much lesser extent. In infants the scalp veins are sometimes used.
A peripheral IV cannot be left in the vein indefinitely, because of the risk of insertion-site infection leading to phlebitis, cellulitis and sepsis
I.V. PAIN MANAGEMENT
One of the most frequent contributors to patient dissatisfaction is painful phlebotomy and IV starts
- Use 25-27g insulin syringe to create a wheal similar to a TB skin test on top of or just to side of vein with 0.1 -0.2 ml normal saline or 1% xylocaine without epinephrine
- Topical anesthesia cream (ie EMLA) may be applied to children>37 weeks gestation 1 hr. prior to stick. It might be a good idea to anesthetize a couple of sites
- Have the patient close their fist (NO PUMPING) prior to stick
- Make sure the skin surface cleansing agent (alcohol/chlorhexidine) is dry prior to stick. Drawing this into the vein may stimulate the vasoconstrictive action of the tunica media layer
POSSIBLE COMPLICATIONS
- Ø Phlebitis (inflammation of vein). Skin over these region is red, painful and hot
- Ø Infiltration (leaking of I.V. fluid into tissues around the vein). These can occur in the accidental dislodgement of catheter and noticeable swelling is seen
CENTRAL LINE
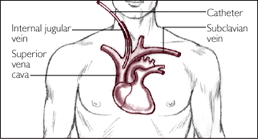
Central IV lines flow through a catheter with its tip within a large vein, usually the superior vena cava or inferior vena cava, or within the right atrium of the heart. This has several advantages over a peripheral IV:
- It can deliver fluids and medications that would be overly irritating to peripheral veins because of their concentration or chemical composition. These include some chemotherapy drugs and total parenteral nutrition.
- Medications reach the heart immediately, and are quickly distributed to the rest of the body.
- There is room for multiple parallel compartments (lumen) within the catheter, so that multiple medications can be delivered at once even if they would not be chemically compatible within a single tube.
- Caregivers can measure central venous pressure and other physiological variables through the line.
CENTRAL LINE CARE / MAINTENANCE
For percutaneous, tunneled and PICC
- Flush after each access or daily for catheters
Adults: 10ml saline
Pediatric/neonates: 5ml saline
- Transparent dressing change
For implanted access
- Flush after each use and weekly while accessed,
- monthly when not acessed
– 10ml saline
– followed by 4.5ml-5ml heparinized saline (100units/ml for adults and 10units/ml for pediatrics )
- Transparent dressing/ access needle change every 7days
Complication and risk
TROUBLESHOOTING
- Vascular access device will not flush/can’t draw blood
– Evaluate for kink in tubing or catheter tip against vein wall.
- Vascular access device (VAD) leaking when flushed
– Verify that hub access cap is connected correctly
- Patient complains of pain while VAD being flushed
– Assess for infiltration
- VAD broken
– PICC’s may be repaired. All other devices must be replaced